Best Male Infertility Treatment in Bangalore.
Book a Free Consultation Now!
Low Sperm Count
A man’s sperm count is considered lower than normal if he has fewer than 15 million sperm per mL of semen which can decrease the chances of conceiving a child simply because of fewer opportunities for fertilization. Low sperm count is caused by a variety of physiological, environmental and lifestyle factors, from infections, hormonal imbalances, and autoimmune problems, to emotional stress, depression and obesity.
Poor sperm movement
Sperm motility refers to the ability of sperm to move efficiently. It is important in fertility because sperm need to move rapidly and directly through the woman’s reproductive tract to reach and fertilize her egg before the sperm cells die. Damage to the testicles, which make and store sperms could be a reason for low sperm motility.
Sperm Quality
Degradation of sperm DNA affects the health of an embryo’s genetic make-up, and can contribute to miscarriage. After men turn 40, the quality of their sperm’s genetic material lessens and the new sperm isn’t as good as the sperm they produced when younger. It’s a natural and irreversible effect of aging, much like how women’s eggs deteriorate after age 35. Declining sperm quality may not impact a man’s ability to ejaculate or successfully fertilize an egg, but it is more likely to make an embryo nonviable.
Structural Issues
Anything that clogs the genital tract can prevent the passage of sperm. This might be the result of a genetic or congenital defect. Infection or inflammation caused by a sexually transmitted disease can also obstruct sperm production. Other reasons include surgical scar tissue or twisted, bulging veins in the scrotum.
Varicocele
Degradation of sperm DNA affects the health of an embryo’s genetic make-up, and can contribute to miscarriage. After men turn 40, the quality of their sperm’s genetic material lessens and the new sperm isn’t as good as the sperm they produced when younger. It’s a natural and irreversible effect of aging, much like how women’s eggs deteriorate after age 35. Declining sperm quality may not impact a man’s ability to ejaculate or successfully fertilize an egg, but it is more likely to make an embryo nonviable.
- Previous prostate inflammation or genital infections
- Testicular injury or twisting (torsion)
- Puberty, either early or late
- High-temperature exposure of the genitals
- Hernia repair
- Testicles that haven't descended
Advancements in the Field of Male Infertility Treatment
Computer Assisted Sperm Analysis (CASA)
A semen analysis is a test performed to screen for male fertility problems. The evaluation of sperm cell motility (movement) and morphology (shape and size) is an essential parameters in the examination of sperm quality and CASA allows an objective assessment of sperm quality. At GarbhaGudi, we use a sophisticated electronic imaging system to visualize the sperm and an advanced software program to evaluate dozens of individual sperm parameters. This examination provides very accurate results and treatment can be specifically tailored for male infertility.

Percutaneous Epididymal Sperm Aspiration (PESA)
PESA is a simple procedure that involves inserting a needle into the epididymis to extract fluid that contains sperm. The aspirated fluid will then be sent to the laboratory for sperm aspiration. The sperms extracted from the epididymis require a procedure called ICSI (intracytoplasmic sperm injection), an IVF procedure where the sperm cell is directly injected into the cytoplasm of the egg. This same-day procedure gives the benefit of not having to make an incision on the body. PESA is one of the most effective and successful techniques of sperm aspiration. If your testes are healthy to produce healthy sperms that are not able to make their way into the ejaculate, this same-day procedure would be considered as it does not involve any surgical incision.

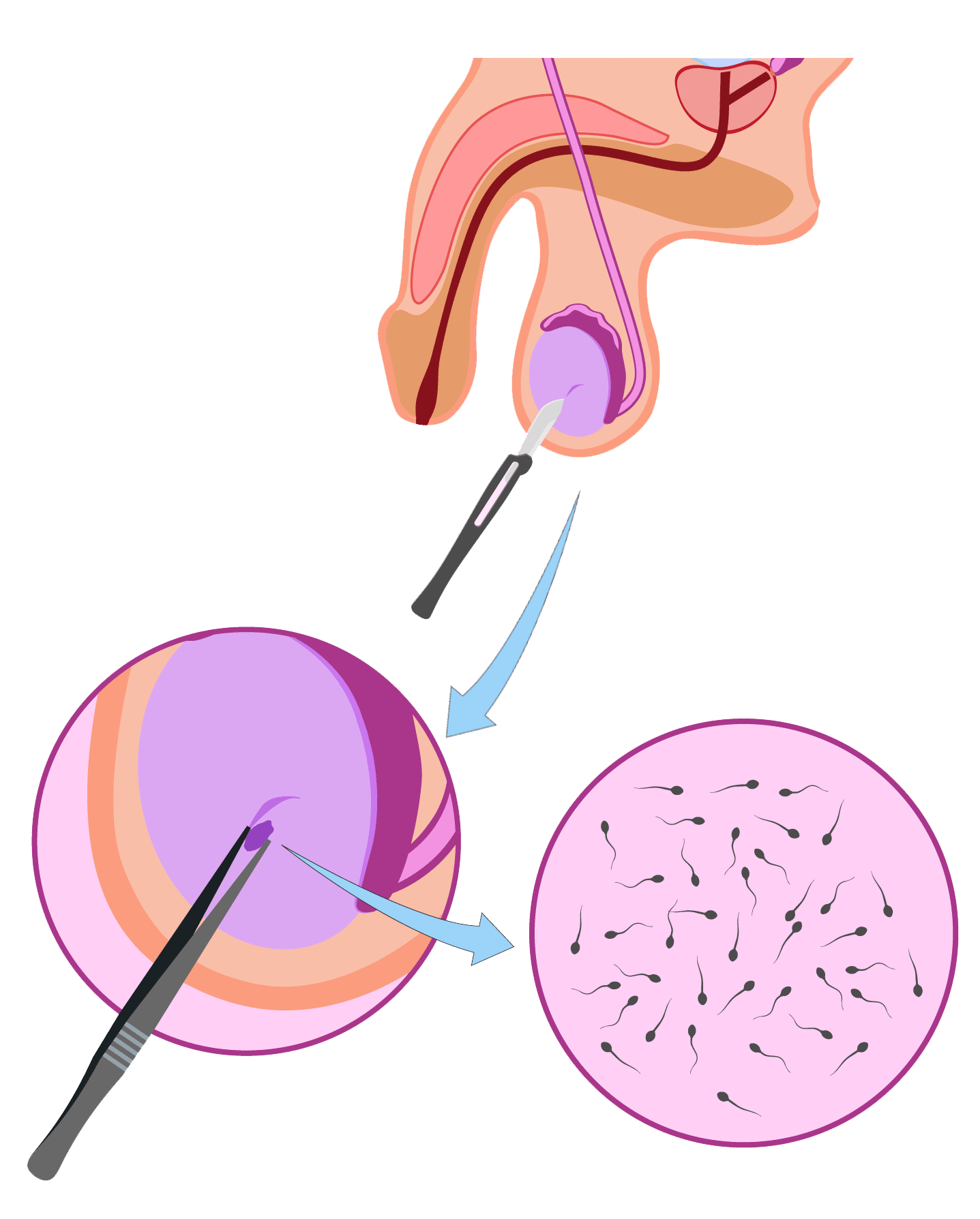
Testicular Sperm Aspiration (TESA)
Similar to PESA, testicular sperm aspiration (TESA) is also one of the newest methods used in the treatment of infertility in men. This technique is widely recommended to men with azoospermia, in which there is a lack of sperm in the ejaculate. The invention of ICSI (intra-cytoplasmic sperm injection) has made it possible for a number of men with azoospermia to biologically father a child. This has been a breakthrough procedure in extracting sperm directly from the testis of a male. The procedure is done by insertion of a needle into the testis and with the aid of negative pressure, fluid and tissue are aspirated. The sample thus obtained undergoes further processing to retrieve the sperm cells in a laboratory. In this procedure, the sperm cells do not have to necessarily be mature and travel through the epididymis in order to fertilize the egg and because the sperms are immature, ICSI has to be performed so as to be able to obtain single sperm and inject straight away into the egg for further fertilization to occur and result in the embryo formation. Both the procedures are helpful in treating the male infertility factor, but there are certain factors to be taken into consideration before deciding which one is ideal for your condition. This is possible only through a fertility specialist. Approach the right facility and choose a specialist who can efficiently guide you through your journey to reach your destination of being a biological father. GarbhaGudi IVF Centre – A path from dreams to success.
Semen Freezing
Semen freezing, commonly known as sperm cryopreservation or sperm banking/freezing, is a method of preserving sperm cells. It is a procedure that uses unique chemical protectants to preserve and store sperm in a sperm bank for future use. Sperms may be kept in liquid nitrogen at -196°C for many years with reasonable quality and be used when needed in the future. Donor sperm can also be collected and stored by sperm banks. Storing your sperm may allow you to use it for future therapy. Frozen sperm (including donor sperm) can thus be used in IVF and IUI in the future.
